Best-in-Class Inpatient RCM Services & Software
RCM Services & Software
Maximize your revenue with Claimocity. Our expert RCM services increase your earnings without extra stress.

RCM Services & Software Built for Inpatient Providers
Maximize your revenue with Claimocity. Our expert RCM services increase your earnings without extra stress.
Billing headaches?
Let’s fix that.
Revenue cycle management shouldn’t be your second job. Between complex coding, constant rule changes, and payer demands, we’ve mastered the chaos, so you don’t have to.
Claimocity handles the heavy lifting with powerful RCM services and smart billing software, so you can focus on what matters most.
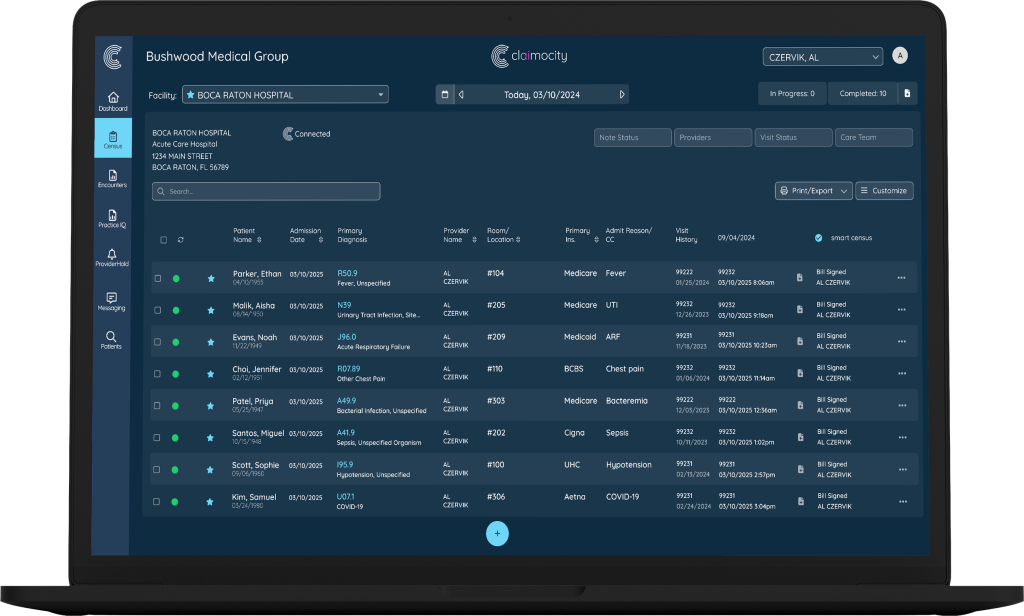
GETTING PAID HAS NEVER BEEN FASTER OR EASIER
Most billing systems slow you down. Ours is made to speed up payments, cut out costly mistakes, and give your day back.
- Expert teams who speak your specialty’s language
- Smart technology that catches issues before they become problems
- Inpatient focus means we understand your unique workflows
- Transparent reporting so you always know where your money is
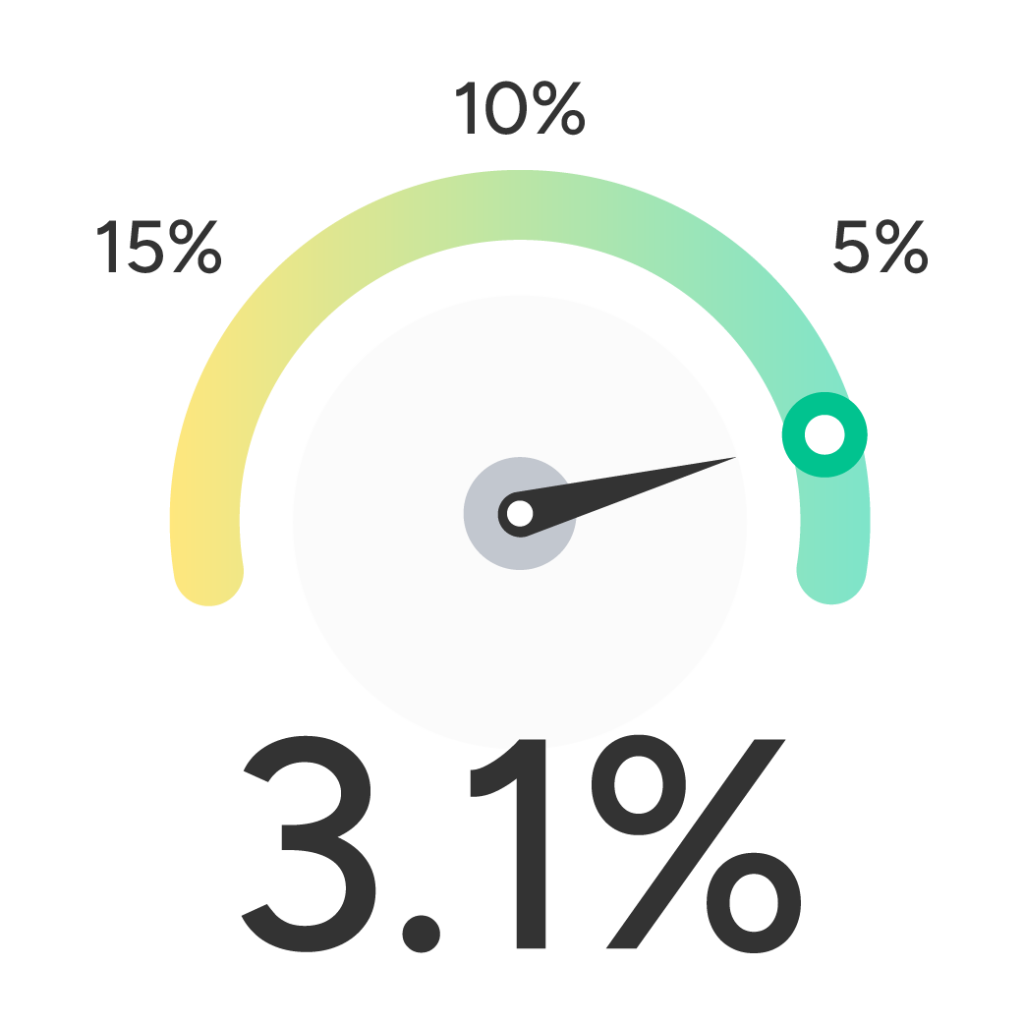
Our Results Speak for Themselves

Revenue Realization Date (Day 90)
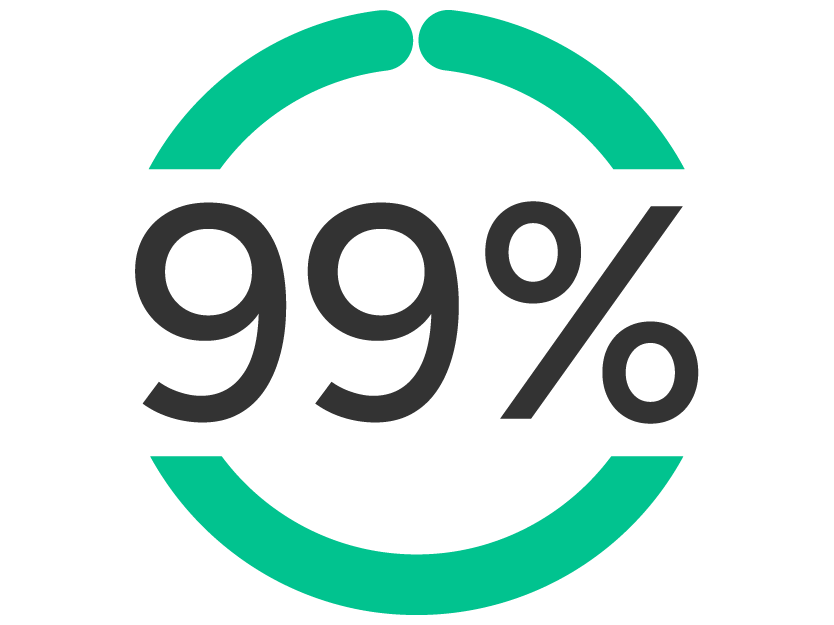
Net Collection Rate (NCR)

Clean Claim Rate
THERE'S MORE
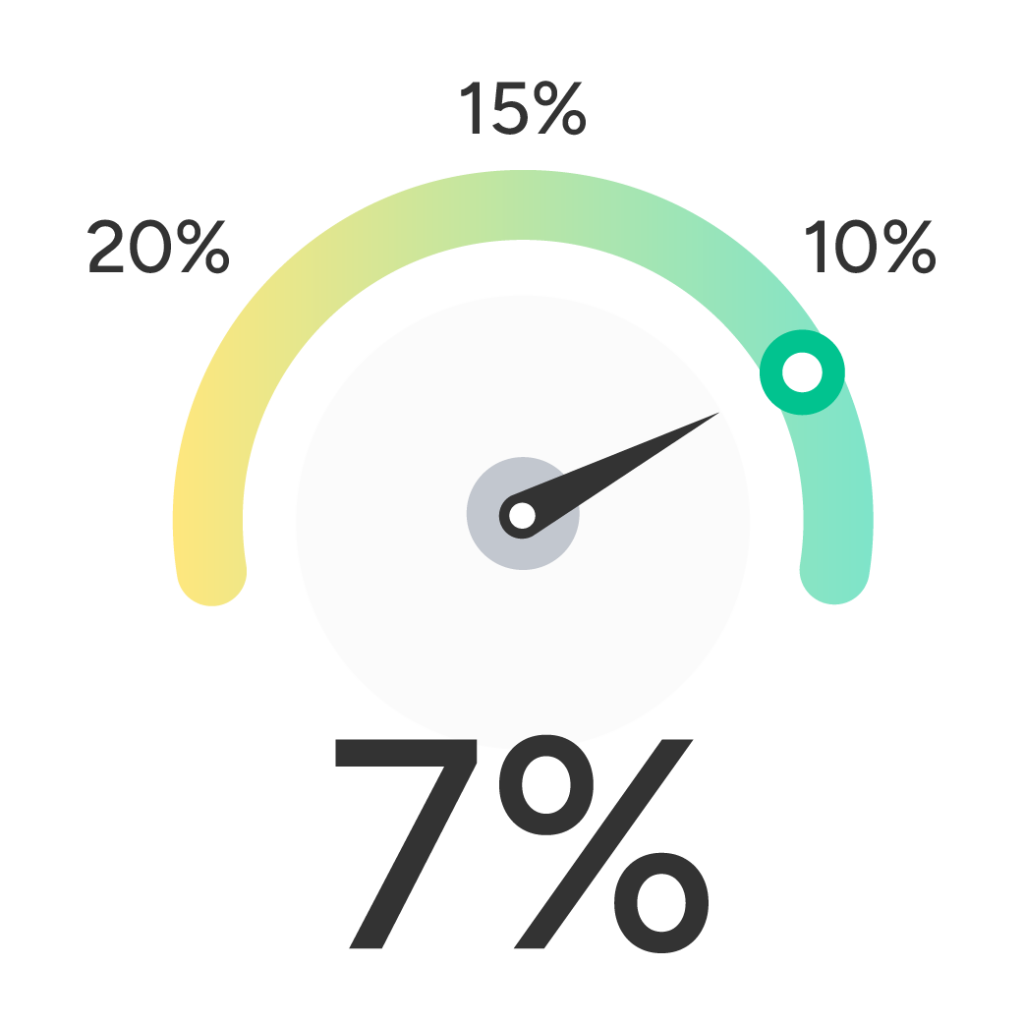
Accounts Receivable > 90 Days
Denial Rate

Days Outstanding Revenue (DOR)

YOUR BENEFITS WITH CLAIMOCITY
- Peace of Mind: Created by industry leaders with 20+ years of experience
- Professional Freedom: Focus on medicine, not medical billing
- Work-Life Balance: Stop thinking about billing errors after hours
COMPLETE RCM SERVICES
Everything your practice needs to get paid, all in one place. No toggling. No bottlenecks. No time wasted.
Claim Submission
Our proprietary claims submission engine moves clean claims to payers faster, reducing potential rejections and denials.
Payment Posting
Timely and accurate posting of insurance payments, copays, and deductibles keeps your AR lean and your cash flow strong.
AR MANAGEMENT
Machine-learning workflows identify errors and potential payment delays before they hurt your bottom line.
DENIALS MANAGEMENT
Denied or underpaid claims get corrected and resubmitted quickly, with pattern tracking to prevent repeat issues.
PATIENT BILLING & COLLECTIONS
From statements to follow-ups, we make billing easy for patients and seamless for your staff.
IN-APP BILLING SUPPORT
Your team can communicate securely directly in the app. So questions get answered quickly and issues get resolved faster.
CREDENTIALING
From onboarding new providers to managing recredentialing, our team ensures your group stays in-network and ready to bill.
REPORTING & ANALYTICS
Know exactly how you're performing and where opportunities exist with detailed dashboards and monthly reports.
Automate Your Day
WHO WE HELP
Our specialized RCM services are designed for the demands of inpatient care. Here are just a few of the specialties we support:
Critical Care
Emergency Medicine
Infectious Disease
Inpatient Psychiatry
Internal Medicine
Physiatry (PM&R)
Surgery
See What Providers Are Saying


Just what we needed."

Services FAQ

DOES CLAIMOCITY OFFER CREDENTIALING SERVICES?
As part of your Billing Team, our Credentialing Specialists expedite the resolution of billing-related issues and deliver faster initial credentialing so new providers can see patients sooner.

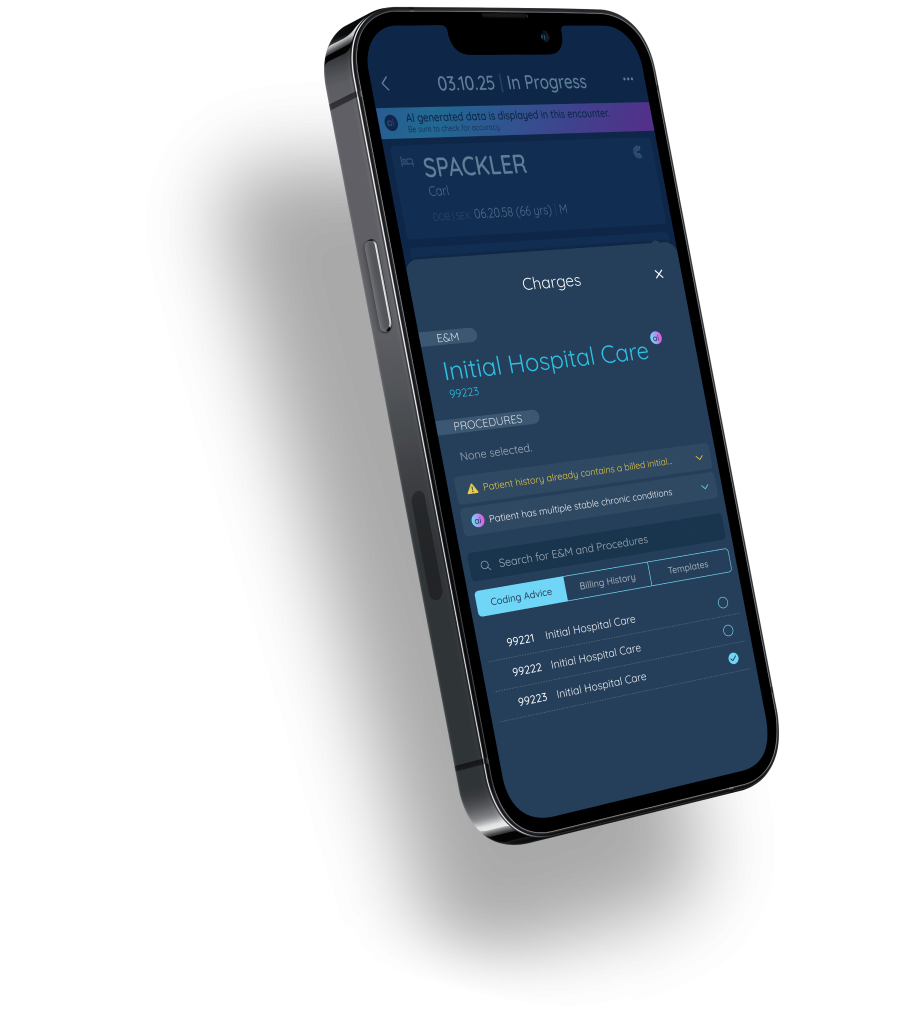
DOES CLAIMOCITY OFFER CODING SERVICES?
In-app, AI-assisted coding support is backed by a team of certified coders who ensure accurate documentation of encounters.

WHAT REVENUE CYCLE REPORTING IS AVAILABLE?
Practice and provider financial health monitoring includes tracking key performance indicators (KPIs), providing detailed monthly summaries and identifying areas for improvement.
Ready to Maximize Your Revenue?
Your current RCM is costing you money. Whether it’s missed charges, slow payments, or administrative overload. You’ve done the work, now it’s time to get paid.
