Claimocity Claims
From Burnout to Balance:
How AI Can Reclaim Your Time as a Hospitalist

The Hospitalist Hustle: Balancing Patients & Paperwork
Being a hospitalist is both demanding and rewarding. You’re on the front lines and delivering critical care to patients around the clock. However, the administrative burden of medical billing can quickly eat away at your valuable time. Hours spent on manual data entry and coding translate quickly leads to provider burnout.
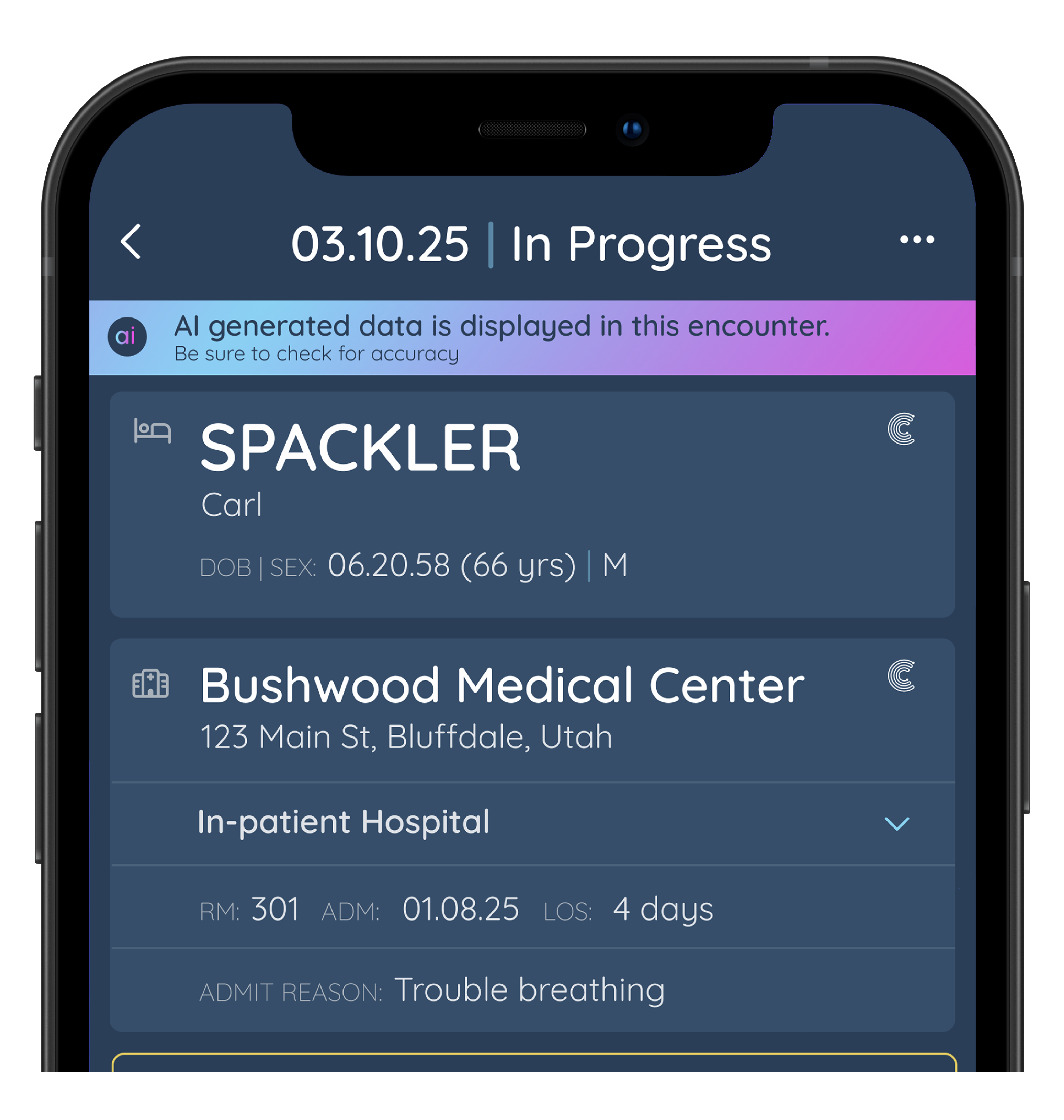
What if there was a way to automate tedious billing tasks, freeing you up to focus on what matters most to you? Claimocity AI Charge Capture leverages the power of artificial intelligence to streamline your billing workflows.
Here's how Claimocity AI can help you reclaim your time:
- Automatic Data Mining: Scans your signed EHR notes, identifying potential charges you might have missed.
- AI-Powered Coding: Analyzes diagnoses and procedures, suggesting accurate ICD-10 and CPT codes, minimizing coding errors.
- Pre-populated Charge Lists: Review and approve billable encounters in a fraction of the time compared to manual entry.
Real Results, More Time for You
After beta testing the initial release of Claimocity AI with our customers, we collected extensive data revealing that providers save an average of 8.75 hours per provider per month, adding up to hundreds of hours saved collectively.
This means more time for:
- Work-Life Balance: Reclaim valuable hours to spend with family, recharge, or pursue personal interests.
- Professional Growth: Stay ahead with continuing education, research, or career development.
- Operational Efficiency: Focus on optimizing workflows, managing teams, and enhancing practice performance
Don’t let medical billing take over your day. Claimocity AI streamlines your workflow, helping you achieve the work-life balance you deserve.
Learn More Here: