Claimocity Claims
What is Charge Capture?
An End-to-End Physician Guide

Summary Points
- Avira Insights revealed that 83% of practices transitioning from subpar charge capture solutions swiftly discovered superior platforms within just 1-2 changes, resulting in an average ROI increase of 7-11% above investment within a concise 16-month period.
- Navicure’s investigation unveiled that 37% of providers grappled with a significant denial rate, while an overwhelming 80% of healthcare providers faced adverse effects from insurance claim denials, citing top reasons such as missing or inaccurate patient data alongside inadequate documentation.
- The Healthcare Financial Management Association (HFMA) unearthed that the typical medical practice hemorrhages approximately $125,000 annually due to deficient charge capture processes.
- Forward-looking 2023 data-science forecasts underscore advanced automation, the expansion of artificial intelligence, and seamless EHR integrations as pivotal areas poised to deliver substantial enhancements in billing productivity and efficiency within charge capture systems.
This is Worth Your Time
This guide is the result of extensive R&D collaboration between experts from various fields, offering a data-driven analysis based on scientific and case studies. It aims to provide readers, from beginners to advanced users, with comprehensive insights and expectations for future changes to optimize decision-making and value.
KEY TERMS REVIEW
Trend Forecasting: Trend refers to the prevailing direction or tendency, while forecasting predicts future occurrences. Trend forecasting involves predicting the evolution and impact of current and upcoming trends.
Medical Revenue Cycle Management (RCM): Medical RCM is the systematic process of managing financial income generation in healthcare. It involves identifying, analyzing, submitting, tracking, reconciling, and collecting payments for healthcare claims.
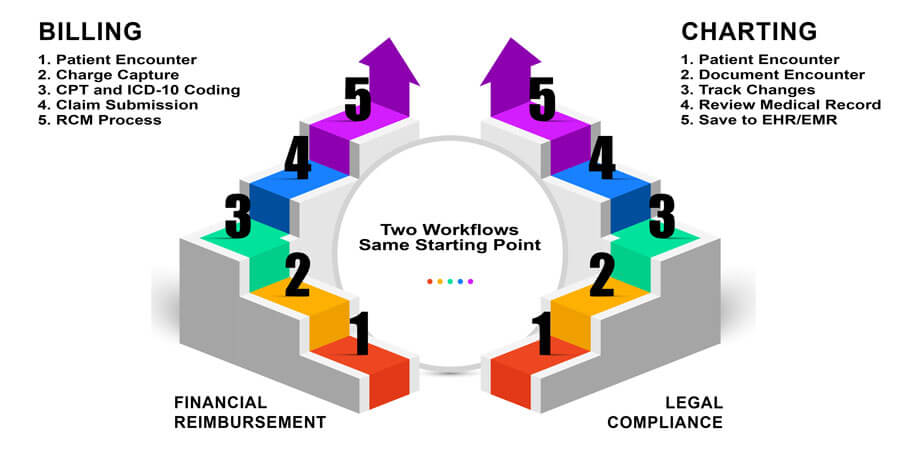
Medical Billing and Coding: Medical billing and coding is the standardized processing of patient encounter data into reimbursement requests and medical records.
Hospitalist and SNFist: Hospitalists provide medical care in inpatient settings like hospitals, while SNFists are hospitalists who primarily work in skilled nursing facilities.
Trending Specialties: Specialties associated with hospitalists and SNFists include internal medicine, critical care, physical medicine and rehabilitation, infectious disease, obstetrics and gynecology, pediatrics, pulmonology, cardiology, neurology, and others.
What is Charge Capture? Physicians use this systematic method to record patient encounters using CPT and ICD-10 codes, initiating the claim submission and billing process for insurance reimbursement.
Variants include:
- Charge Capture Specialist
- Healthcare Charge Capture
- Charge Capture Revenue Cycle
- Hospital Charge Capture
- Charge Capture Audit
- Medical Charge Capture
- Mobile Charge Capture
- Physician Charge Capture
Notably, “charge capture audit” stands out as it involves a comprehensive review of the end-to-end process to identify issues and successes objectively. A proficient billing team and charge capture support system should handle this, positively impacting A/R efficiency and providing valuable feedback to providers.

Trends and Forecasts
Medical trend analysis is used as a means of forecasting key industry trends to predict opportunities, uncover potential issues, and enable a greater level of strategic decision-making.
Current Charge Capture Trends:
- Billing automation: Healthcare organizations are increasingly using automated charge capture systems to reduce errors and improve efficiency. These systems use technology such as artificial intelligence and machine learning to analyze clinical documentation and identify chargeable items.
- Mobile Technology: With the rise of mobile technology, healthcare providers are using mobile devices to capture charges on the go. This allows them to capture charges in real-time, which can help reduce billing errors and improve revenue.
- Integration with electronic health records (EHRs): Many charge capture systems are integrated with EHRs, allowing for seamless communication between clinical documentation and billing. This helps to reduce errors and improve accuracy in charge capture.
- Emphasis: on documentation compliance: With increasing regulatory requirements, healthcare organizations are placing a greater emphasis on compliance in charge capture. This includes ensuring that charges are accurately and appropriately documented, and that billing follows relevant regulations.
- Data analytics: Healthcare organizations are using data analytics to identify trends and patterns in charge capture, and to optimize billing processes. This can help to improve revenue and reduce billing errors over time.
- Charting: automation: With the help of technology, charge capture is becoming more automated. Electronic health record (EHR) systems and other software can identify services provided and help ensure that they are accurately documented and billed.
- Real-time documentation: Charge capture is becoming more real-time. Physicians and other healthcare providers are documenting services and procedures as they are provided, rather than waiting until later to enter the information. This helps to ensure that nothing is missed, and that billing is accurate.
- Analytics: Healthcare organizations are using analytics to identify areas where charge capture can be improved. For example, data analysis can help identify services that are frequently missed or under-billed.
- Increased focus on coding compliance: With increased scrutiny from regulators and payers, healthcare organizations are placing a greater emphasis on compliance with billing regulations. This includes ensuring that charges are appropriately coded, and that billing is consistent with levels that don’t generate under coding or over coding audit risks.
- Integration with quality improvement processes: Charge capture is increasingly being integrated into other healthcare processes, such as clinical decision support and quality improvement initiatives. This helps to ensure that billing is aligned with overall healthcare goals and that services are appropriately documented and billed.
Data Science Forecasts
- Increased focus on physician satisfaction scores and mental health: Physician burnout and mental health is coming into increasing focus as analytics measuring professional satisfaction, happiness levels, and work-life balance are corresponding to levels of productivity, patient care, readmission rates, accurate diagnostics, patient satisfaction, and treatment quality metrics.
- Higher levels of rounding automation: The current focus on billing and charting puts entirely too much pressure on providers to navigate complex non-medical requirements at the expense of the quality of care. Greater technological increases focused in these areas will begin to shift this pendulum in the other direction, freeing doctors more to focus on the medicine.
- Increased adoption of artificial intelligence (AI) and machine learning (ML): As healthcare organizations continue to seek ways to improve charge capture accuracy, AI and machine learning could play an increasingly important role. These technologies could be used to automatically identify services provided and ensure that charges are accurately captured.
- Continued emphasis on compliance: With the increasing scrutiny on billing practices, healthcare organizations will likely continue to prioritize compliance with billing regulations. This could include investing in training for healthcare providers and support staff to ensure that they are familiar with billing rules and guidelines.
- Greater integration with revenue cycle management: Charge capture will continue to be an important component of the revenue cycle management process. As such, healthcare organizations will likely seek to integrate charge capture with other revenue cycle functions, such as claims processing and payment posting.
- Use of predictive analytics: Predictive analytics could be used to forecast potential revenue loss due to missed charges and identify areas where charge capture could be improved. This could help healthcare organizations proactively address potential issues and ensure that charges are accurately captured.
- Increased focus on patient engagement: As patients take on a greater role in their own healthcare, charge capture could become more patient-centric. For example, healthcare organizations may seek to provide patients with greater visibility into the services provided and the associated charges, as well as tools to help them understand their insurance benefits and out-of-pocket costs.

Paper vs Electronic/Mobile Process
Paper charge capture in healthcare, dating to early medicine, once relied on manual forms like progress notes and lab reports. Standardization came with the introduction of the Healthcare Common Procedure Coding System (HCPCS) in the 1980s, simplifying billing. With the rise of electronic health records (EHRs) in the late 1990s and early 2000s, many shifted to electronic systems, citing efficiency and accuracy benefits. Today, electronic systems dominate, though some still use paper. Administrative tasks consume much of physicians’ time, impacting patient care and billing efficiency. Accurate charge capture is crucial to avoid preventable denials.
Benefits of Great Mobile Charge Capture
- Fast Turnarounds: Helps rounding physicians save time on the front-end submission process and get paid faster on the backend claim processing process.
- Automations: Automates segments of the workload that can be derived contextually from other areas, handled by smart software, or handled effectively by trained support staff.
- Point of Care Productivity: Reduces end of day and end of week workloads by streamlining the necessary efforts into the rounding processes and enabling greater productivity in less time at or between patient encounters.
- Generating Chart Notes: At the very forefront of the charting efficiency trend is the ability to concurrently generate chart notes in the same workflow as submitting coded claims for billing. The efficiency factor is exponentially larger as it handles two critical time sucks in one workflow.
- Messaging Securely: HIPAA compliant texting enables rounding physicians to communicate effectively within their group while maintaining the security of the information being transmitted—protected health information.
- Coordinated Care: This can mean creating and managing custom care teams to cover rounds across multiple facilities and patient needs, or it can mean enabling providers to more effectively care for patients who are also being seen by other covering physicians.
- Coding Efficiency: Lower coding averages always means revenue left on the table and higher coding averages means increased risks of audits that have severe legal and financial ramifications even when successful. Identifying and rectifying inaccurate coding patterns can help protect providers and practices against risks.

Peak Charge Capture Performance
Achieving peak performance in medical charge capture process is critical for accurate billing and efficient revenue cycle management. Here are some tips that can help improve the charge capture performance in the medical setting:
- Standardize Charge Capture Processes: Establishing standardized processes for charge capture can reduce errors and ensure consistent performance across providers and departments. Consider implementing electronic charge capture systems to streamline the process and reduce manual errors.
- Employ User-Friendly Tools with Good UI/UX: Ensure that the tools are as user friendly as possible and all providers and staff members receive comprehensive training on charge capture processes, including coding requirements and documentation standards. Ongoing training and refresher courses can help ensure that everyone is up to date on the latest practices and requirements.
- Conduct Regular Audits: Conduct regular audits of charge capture processes to identify and correct any issues or errors. Use data analytics and reporting tools to monitor performance and identify areas for improvement.
- Utilize Technology: Utilize technology to automate charge capture processes and reduce manual errors. Consider implementing electronic health records (EHRs), coding tools, and charge capture software to improve accuracy and efficiency.
- Encourage Collaboration: Encourage collaboration between clinical and billing staff to ensure that all charges are captured accurately and efficiently. Consider establishing cross-functional teams to identify and address any issues or inefficiencies in the charge capture process.

Challenges in the Charge Capture Process
Research shows traditional paper charting is highly inefficient compared to electronic medical or health records. Despite this, 27% of healthcare organizations still use paper charge capture systems according to a 2019 Healthcare Finance article. Physicians relying on index cards or hospital printouts for notes and charges face ineffective billing and coding procedures. Common challenges with traditional paperwork include:
ICD-10 Code Inaccurate Diagnosis
An inaccurate ICD-10 code diagnosis can have significant negative consequences for healthcare providers, patients, and payers. Here are some potential impacts of inaccurate ICD-10 code diagnosis:
- Revenue loss: Inaccurate ICD-10 code diagnosis can lead to incorrect billing, which can result in revenue loss for healthcare providers.
- Compliance risks: Inaccurate ICD-10 code diagnosis can also lead to compliance risks, such as billing errors and incorrect coding. This can result in audits, fines, and other legal issues.
- Delayed or denied reimbursements: Payers may deny or delay reimbursement for services if the ICD-10 code diagnosis is inaccurate, which can impact cash flow and financial performance.
- Reduced quality of care: Inaccurate ICD-10 code diagnosis can lead to inappropriate treatments and procedures, which can negatively impact patient outcomes and quality of care.
- Legal liabilities: Inaccurate ICD-10 code diagnosis can also result in legal liabilities if patients are harmed because of incorrect diagnoses or treatments.
Healthcare providers can prevent inaccurate ICD-10 code diagnoses by mastering the coding system, staying updated on changes, and employing validation processes. Electronic health record systems and regular audits aid in accurate coding and billing, identifying and resolving potential issues.
Missed Charges
Missed charges can significantly impact healthcare organizations, both in revenue loss and compliance risks. Here are some facts about missed charges in the charge capture process:
- Common problem in healthcare: According to a study by the Healthcare Financial Management Association, the average hospital misses about 3% of chargeable services, which can result in significant revenue loss over time.
- Compliance risks: Failure to capture charges accurately can result in compliance risks, such as billing errors and incorrect coding. This can lead to audits, fines, and other legal issues.
- Can be caused by a variety of factors: Missed charges can be caused by a variety of factors, such as poor documentation practices, lack of training, and inadequate charge capture technology.
- Difficult to detect: Missed charges can be difficult to detect, as they often go unnoticed until a comprehensive audit is conducted. This can result in lost revenue that cannot be recovered.
- Technology can help reduce missed charges: Technology, such as electronic charge capture tools, can help reduce the incidence of missed charges by automating the charge capture process and providing real-time feedback on charge accuracy.
- Regular monitoring and audits can help identify missed charges: Regular monitoring and audits of the charge capture process can help identify missed charges and other areas for improvement. This can help ensure that the charge capture process is operating at peak performance and that revenue is being captured accurately.
Erroneous Charges
Erroneous charges in the charge capture process can lead to revenue loss, compliance risks, and patient safety concerns. Here are some facts about erroneous charges in the charge capture process:
- Significant issue: According to a study by the Healthcare Financial Management Association, the average hospital experiences an error rate of 3-5% in its charge capture process. This number rises to an average of 8-9% for medium to large private practices and 11-13% for solo practitioners and small practices.
- Revenue loss is very real: Erroneous charges can result in revenue loss, as services that are not properly documented and charged cannot be billed to payers.
- Compliance issues with legal and financial risks: Erroneous charges can also result in compliance risks, such as billing errors and incorrect coding. This can lead to audits, fines, and other legal issues.
- Poor documentation practices are a common cause of erroneous charges: Poor documentation practices, such as incomplete or inaccurate medical records, can lead to erroneous charges.
- Technology can help reduce erroneous charges: Technology, such as electronic charge capture tools and automated billing systems, can help reduce the incidence of erroneous charges by improving the accuracy of the charge capture process.
- Regular monitoring and audits can help identify erroneous charges: Regular monitoring and audits of the charge capture process can help identify erroneous charges and other areas for improvement. This can help ensure that the charge capture process is operating at peak performance and that revenue is being captured accurately.
- Erroneous charges can also pose patient safety concerns: Erroneous charges can lead to incorrect treatments or procedures being performed, which can pose patient safety concerns. It is important to ensure that the charge capture process is accurate and reliable to prevent these types of errors.
Charge Lag
Charge lag is the delay between healthcare services and billing entry, affecting revenue cycle management. Longer charge lags can lead to delayed reimbursement and revenue loss. Factors like service complexity and documentation affect charge lag length. Shorter charge lags are preferable for timely reimbursement and reduced lost charges risk.
Rounding and Face Sheets
Face sheets are concise patient summaries printed at hospitals, handed to rounding physicians. Integrating new patient data into charge capture platforms is often inefficient. Studies reveal frustration among hospitalists due to redundant data entry, as EHR information fails to sync with billing software.
Manual Data Entry, Redundancy, and Organization
These are all related and I discuss them further in a separate guide. A physicians weekly required workload of clerical and administrative burdens including manual data entry, redundant data entry, and disorganized paperwork is a massive issue for a wide variety of key variables that impact physician production and cap practice growth.

AI/ML in Charge Capture Billing and Coding
Artificial Intelligence (AI)
The evolution of AI technology helps in charge capture by accelerating the process and billing workflow with fewer missing claims, quicker results, higher benchmarks, and financial metrics. Recent improvements to AI-supported mobile charge capture software helps further eliminate errors, denials, and missed charges.
Machine Learning (ML)
Machine learning, a subset of artificial intelligence, employs algorithms to analyze medical data, predict outcomes, diagnoses, treatments, and billing patterns. Through extensive medical data training, it identifies errors, missing information, and data patterns. Medical machine learning promises accurate diagnoses, personalized treatments, and better patient outcomes. Ethical development and usage, alongside privacy safeguards, are crucial for ensuring algorithm reliability and patient privacy.

The Importance of Integrations
Integrations are crucial for charge capture systems, as poor ones lead to information flow issues, errors, and redundant work. Seamless interoperability with practice and billing software, as well as EHRs, is essential for accuracy, efficiency, and revenue generation. However, integrating with hospitals and facilities is challenging due to their unique systems. Effective integration ensures data pulls and pushes seamlessly between systems, optimizing workflow. While most charge capture systems claim integration, the quality varies significantly, impacting workload efficiency.
Time Management, Revenue Generation, and Efficiency
Efficient charge capture correlates positively with time management, revenue, and workflow efficiency. Quick billing and coding generate higher revenue in less time, potentially allowing for more patient care or encounters. However, accuracy is crucial; efficiency without accuracy wastes time. Pairing efficiency and accuracy with an organized system leads to increased revenue, better work-life balance, and improved outcomes.
Common Myths and Misconceptions
Paper-Based Charge Capture is Easier
Paper-based billing has been proven in dozens of studies to lead to a measurable percentage of lost charges and misplaced notes, typically between 4-6%. While electronic charge capture has its own set of issues, paper-based processes add unnecessary burdens to the claim submission process.
Billing Lag is Inevitable
Using AI-powered charge capture can significantly reduce billing lag times. Rounding physicians will have the facility to search for the right CPT codes for the services rendered and enter the claims for reimbursement with the single touch of a button from their smartphone or tablet. The faster the billing cycle, the more streamlined the process is with AI-enabled charge capture.
Charge Capture Complicates the Use of PM & EHR’s
In fact, AI charge capture simplifies the process where rounding physicians can easily find the CPT codes and eliminates the manual search of files, redundant entry of information, disorganized workflow, and poor processes that overflow administrative burden for the physicians into other connected systems.
Costs a Lot of Time, Money, and Effort to Implement or Change
If doctors and practice managers could compare two charge captures equally, it would be very easy to decide between them. Unfortunately, there is a level of time, effort, money, and risk involved.
Perception: The decisionmaker does not know whether they are trading one set of problems for another, whether the new solution will end up worse than the last, whether the time and effort sourcing the new solution will generate positive ROI, whether the end user will end up disliking the pick, whether they will be able to easily and effortless learn and intuit the layout and structure of the new tools. And so on.
Reality: According to a 2022 internal study, anonymous for privacy reasons, in 83% of the cases studied, the ROI on the end solution selected was 7-13% higher than the cost of the time, effort, and investment. The caveat was that practices had to switch an average of 3 times before achieving their top level result. So, while switching solutions isn’t ideal and make require not one but two jumps, the data shows that it is a smart move nearly 9 out of 10 times and generates a significantly positive return on investment.

Chosing the Right Solution
23 Tips to Finding a High Performing Charge Capture System
- Easy access at your fingertips and well organized for fast efficient usage
- Voice recognition technology can be a massive time saver on the go.
- Strong OCR that enables data import when taking pictures documents that need to be entered.
- An integrated and organized central census that aligns rounding needs efficiently.
- A powerful set of real-time and real-world analytics and reporting features.
- Intelligent ICD-10 code search that produces the right answers from a wide array of possible inputs/angles.
- Mobile technology capable of high cross-device efficiency on smart phones, tablets, laptops, and desktops.
- Strong automation, custom rules engine, and integrated learning to improve efficiency.
- An array of well-defined time saving features beyond the basics of a mobile app.
- A smartly designed UI/UX system built with the end user in mind that is appealing, easy to learn, and easy to use.
- The ability to receive notifications of new admissions for accurate coverage.
- Personalized care team management to increase care coordination overlap.
- Charting assistance to reduce clerical and administrative burdens.
- Practice management features and/or integrations to handle administrative needs.
- KPIs, benchmarking, peer rankings, and practical analyses for growth.
- A means of securely communicating protected data between providers for coverage.
- Tools designed to improve, identify, or automate solutions relating to coding efficiency issues.
- High financial transparency for claim processing, tracking, and reimbursement analyses.
- The ability to track earnings in real time and manage compensation formulas.
- An effective solution that translates from solo/small practices to large/enterprise clients.
- Pattern analysis features in the software to improve the accuracy and processing speed of the systems.
- Smooth workflows to enable physicians to work at multiple, and often competing tasks, in an organized manner.
- Data integration tools like a patient QR code scanner to reduce clerical tasks.
Scientific Studies & Case Studies Referenced
Scientific Studies Referenced
- Journal of Healthcare Information Management (2006): The Journal of Healthcare Information Management published a study in 2006 found that electronic charge capture reduced billing errors and improved revenue capture compared to paper-based systems. The study concluded that electronic charge capture systems could significantly improve revenue capture and billing accuracy.
- Journal of Hospital Medicine (2011): This exploration aimed to determine whether a hospitalist-specific charge capture system could measurably and significantly improve revenue capture and physician satisfaction. The study found that the hospitalist-specific charge capture system improved revenue capture and physician satisfaction compared to a non-hospitalist charge capture system. This included paper charge capture and electronic charge capture for physicians who are not hospitalists. Journal of American Medical Association (2018) Describing the definition and responsibilities of a SNF-ist, or SNFist, or Skilled Nursing Facility Hospitalist, who mostly practice in the nursing home or associated facilities.
- Journal of Hospital Medicine (2019): A more recent study published in the Journal of Hospital Medicine in 2019 found that electronic charge capture systems were associated with increased revenue capture and decreased time spent on billing compared to paper-based systems. The study also found that electronic charge capture systems were associated with increased physician satisfaction and decreased administrative burden.
- Journal of Hospital Medicine (2019): This study examined the use of a charge capture audit tool or process to improve hospitalist billing accuracy. The study found that the use of a well-designed audit tool led to improved billing accuracy and increased revenue capture.
- Journal of General Internal Medicine (2020): Aiming to identify factors that impact hospitalist charge capture performance, this scholarly article found that factors such as physician experience and workload, as well as the presence of clinical documentation improvement programs, can impact charge capture performance.
- Journal of Medical Systems (2020): Another study published in the Journal of Medical Systems in 2020 compared the accuracy and efficiency of paper-based charge capture to electronic charge capture in a pediatric emergency department. The study found that electronic charge capture was associated with increased accuracy and efficiency compared to paper-based systems.
Case Studies Referenced
- Case study 1: Hospital A hospital in California discovered that they were losing significant revenue due to missing charges for surgical supplies. The hospital implemented a charge capture system that involved barcoding surgical supplies and scanning them during surgery. This system improved charge capture accuracy, resulting in a 30% increase in revenue.
- Case study 2: Cardiology Practice A cardiology practice in Texas discovered that they were missing charges for certain services, resulting in a loss of revenue. The practice implemented a charge capture system that involved automated charge capture software and provider education. This system improved charge capture accuracy and resulted in a 15% increase in revenue.
- Case study 3: Medical Center A medical center in New York discovered that they were missing charges for inpatient stays due to poor documentation. The medical facility implemented a charge capture system that involved training providers on accurate documentation and coding. This system improved charge capture accuracy and resulted in a 25% increase in revenue.
- Case study 4: Physician Private Practice A physician practice in Florida discovered that they were losing revenue due to missed charges for medication administration. The practice implemented a charge capture system that involved using electronic health records (EHRs) to capture charges for medication administration. This system improved charge capture accuracy and resulted in a 20% increase in revenue.
- Case Study 5: Large Academic Medical Center A large academic medical center implemented a charge capture improvement project that involved staff education, process redesign, and technology upgrades. The organization discovered that many of their charges were not being captured or were being captured inaccurately, resulting in lost revenue. Through the project, the organization was able to improve charge capture accuracy by 95%, resulting in a $3 million increase in annual revenue.
- Case Study 6: Community Hospital A community hospital identified a problem with charge capture in their Emergency Department (ED) services. The organization found that many ED services were not being accurately documented or charged for, leading to lost revenue. The hospital implemented an automated charge capture system that integrated with their electronic health record (EHR) system. As a result, the hospital was able to improve charge capture accuracy by 80%, resulting in a $500,000 increase in annual revenue.
- Case Study 7: Charge Capture Platform A branch of the Avira Insights research department performed a study on 1200 practices in specialties dependent on charge capture who see 50% or more of their encounters in acute care, step down, rehab, psychiatric, skilled nursing or other hospital or facility settings. The results showed that on average the practice had to make 1-3 switches to achieve a high performing result, defined as ROI above 5% within 12 months.
- Case Study 8: Private Medical Practice A private medical practice discovered that they were losing revenue due to inaccurate charge capture for ancillary services, such as laboratory tests and radiology services. The practice implemented a charge capture improvement project that involved staff education and process redesign. The practice also implemented an automated charge capture system that integrated with their EHR system. Through these efforts, the practice was able to improve charge capture accuracy by 90%, resulting in a $100,000 increase in annual revenue. Case Study 9: Large Hospitalist Group A large hospitalist group discovered that they were losing revenue due to inaccurate charge capture for their services. The group implemented an electronic charge capture system that integrated with their electronic health record (EHR) system. Through the system, hospitalists were able to accurately document and charge for their services in real-time. As a result, the group was able to improve charge capture accuracy by 95%, resulting in a $1 million increase in annual revenue.
- Case Study 10: Community Hospital A community hospital identified a problem with charge capture for hospitalist services. The hospital found that many hospitalist services were not being accurately documented or charged for, leading to lost revenue. The hospital implemented a charge capture improvement project that involved staff education, process redesign, and technology upgrades. The hospital also implemented an automated charge capture system that integrated with their EHR system. Through these efforts, the hospital was able to improve charge capture accuracy by 80%, resulting in a $500,000 increase in annual revenue.
- Case Study 11: Academic Medical Center An academic medical center discovered that hospitalists were not accurately documenting and charging for their services. The medical center implemented a charge capture improvement project that involved staff education and process redesign. The medical center also implemented an automated charge capture system that integrated with their EHR system. Through these efforts, the medical center was able to improve charge capture accuracy by 90%, resulting in a $2 million increase in annual revenue.


