Claimocity Charge Capture
Our integrated software and services platform addresses all the backend functions your practice needs from capturing patient encounters to getting paid.
Claimocity Charge Capture
Our integrated software and services platform addresses all the backend functions your practice needs from capturing patient encounters to getting paid.

The Industry-Leading Application
Effortlessly manage patient encounters and ensure seamless payment processing. Now powered by AI.
User Friendly
Quicker to Bill
Configurable to
Any Workflow
Everything in
One Platform
Unlock Your Potential With
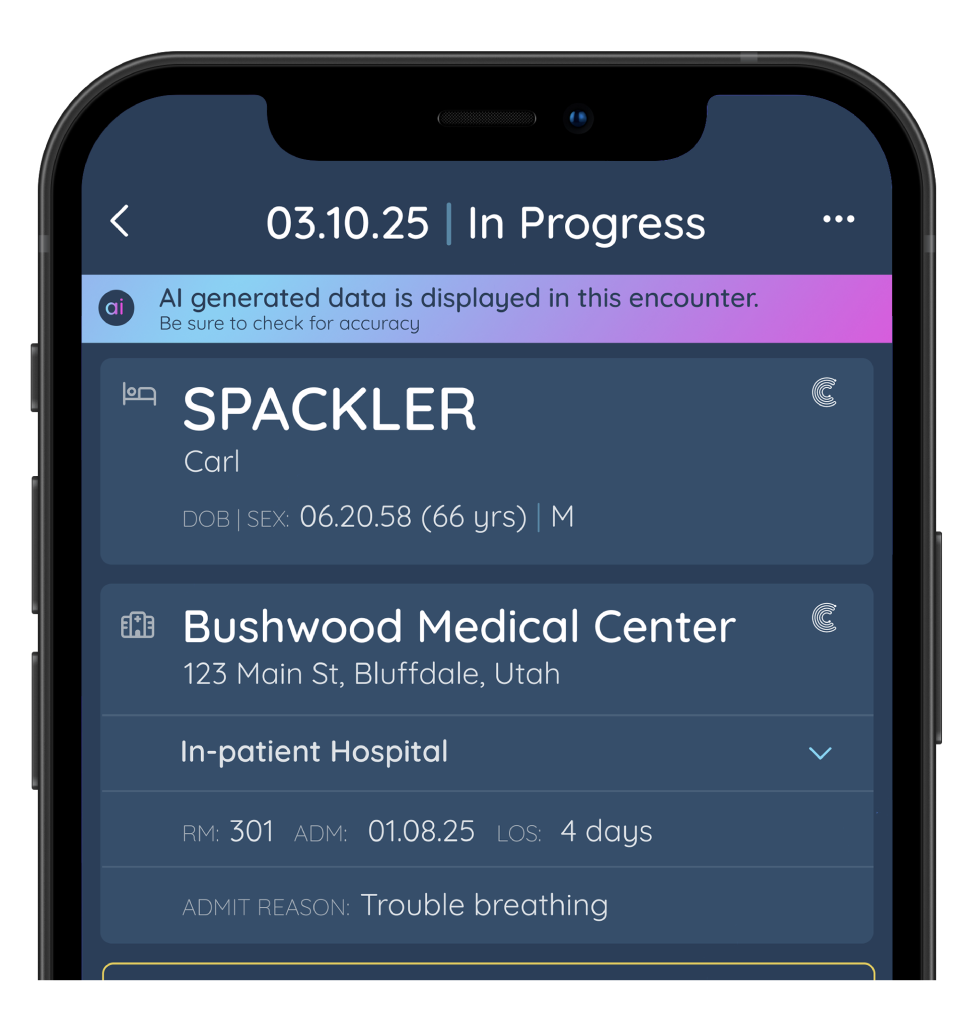
AI Charge Capture
Revolutionize your inpatient practice with our new AI Charge Capture solution. Artificial Intelligence will help save you countless hours by automating your billing process.
INPATIENT CENSUS AND BILLING PLATFORM AT YOUR FINGERTIPS
Our Smart Census is your intelligent organization tool for all your rounding workflows. This personalized hub features a user-friendly interface, integrated data flows, new admission tracking, patient updates, incomplete encounters, missed visit alerts, visit cloning, coding support, billing and more.

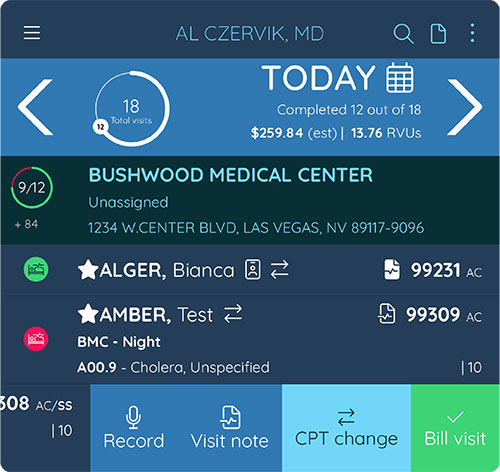
Smart census
- Automated, daily seeding of new & follow-up patients
- Bill patients directly from the census
- One-click SALT (same as last time) Billing
- Billing code predictions
Simplifying the Provider Experience

- Coding Rules Engine
- Patient Encounter History
- Favorite Codes & Patients
- Patient & Encounter Statuses
- Quick Diagnosis Lookup
- Printable Census
Revenue-Centered Tools
Encounter Workbench
Easily review your daily work queue and to-do lists.
Missed Visit Reconciliation
Our platform proactivity reconciles patient visits versus billing to ensure you capture every billable encounter.
Fully Integrated Billing Support
Approved encounters go directly to the billing team queue, allowing providers to communicate with them through in-app messaging.
Practice IQ Activity Dashboard
Access real-time data on charges, revenue, compensation, and KPIs to track your practice’s success.
Practice Workflow Possibilities
Claimocity is fully configurable to accommodate your practice’s unique workflows from managing provider teams to overseeing clinical compliance initiatives.











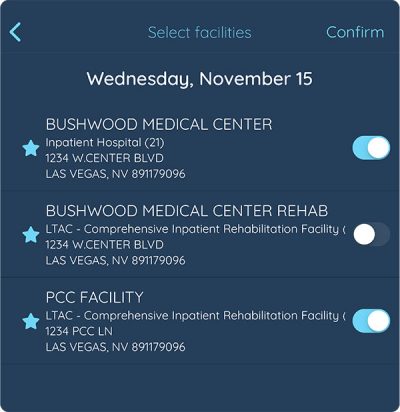
FACILITY CONNECTIVITY
- Census data seeding (when available)
- HL7 ADT and ORU feeds accepted
- Patient demographics
- Facility clinicals
- Access all data to code and bill