
Getting Paid Has Never Been Easier
#1 RANKED HOSPITALIST BILLING SERVICES
- Collect What You Are Owed
- Get Reimbursements Faster
- Avoid Unnecessary Audits
- Highest Reimbursement Rates
- 100% Transparency
- Track Your Claims and Payment Values
- Revenue-Side Peace of Mind
- Business Intelligence Reporting

Getting Paid Has Never Been Easier
#1 RANKED
HOSPITALIST BILLING SERVICES
- Collect What You Are Owed
- Get Reimbursements Faster
- Avoid Unnecessary Audits
- Highest Reimbursement Rates
- 100% Transparency
- Track Your Claims and Payment Values
- Revenue-Side Peace of Mind
- Business Intelligence Reporting
BUYER’S GUIDE - INSIDER MEDICAL BILLING
Choosing to outsource your medical billing department is a major financial decision
for your practice. We offer detailed insights, guiding you through the process and connecting you with a potential partner suited to your practice’s unique needs.
BUYER’S GUIDE -
INSIDER MEDICAL BILLING
Choosing to outsource your medical billing department is a major financial decision for your practice. We offer detailed insights, guiding you through the process and connecting you with a potential partner suited to your practice’s unique needs.
BETTER HOSPITALIST MEDICAL BILLING SERVICES
Nearly all practice management software and billing solutions are designed for doctors working in medical offices and clinics. We thought it time this changed in a big way with solutions designed specifically for you.

- Over a 98% first pass acceptance (average is 70-90%)
- Expert claim tracking and accurate adjudication
- AI-enhanced workflows
- Prompt claims submission
- Automated quality control checks
- Real-time data transparency
- Provider coding efficiency measurements and benchmarking

- Over a 98% first pass acceptance
(average is 70-90%) - Expert claim tracking and accurate adjudication
- AI-enhanced workflows
- Prompt claims submission
- Automated quality control checks
- Real-time data transparency
- Provider coding efficiency measurements and benchmarking
Claimocity offers a unique blend of modern software with revenue cycle experts focused exclusively on the hospital and facility-based physician communities.
Claimocity offers a unique blend of modern software with revenue cycle experts focused exclusively on the hospital and facility-based physician communities.
DENIAL MANAGEMENT IS WHERE OTHERS FALL SHORT
Claimocity strives to submit clean claims, minimizing the chances of denials. Despite the intricacies of revenue cycle management, occasional denials are inevitable. Our skilled management excels in investigating and appealing denied claims, ensuring the capture of this revenue for your practice.

- Our expert team is able to quickly identify and resolve AR stuck points
- Machine learning analyzes denial trends to reduce billing errors
- We provide a physician improvement feedback loops
- AI-Enhanced robust billing rules engine
- Complete denials, appeals, and underpayment management
- Claim scrubbing
- Staying on top of changing regulations and compliance challenges
- Real time, insightful provider and practice reporting

- Our expert team is able to quickly identify and resolve AR stuck points
- Machine learning analyzes denial trends to reduce billing errors
- We provide a physician improvement feedback loops
- AI-Enhanced robust billing rules engine
- Complete denials, appeals, and underpayment management
- Claim scrubbing
- Staying on top of changing regulations and compliance challenges
- Real time, insightful provider and practice reporting
Unpaid claims have the potential to impede your practice, drawing focus and resources away from patient care and crucial healthcare delivery facets. Let us assist you in mitigating and resolving accounts receivable and claim denials, safeguarding your financial stability, reputation, and operational efficiency.
Unpaid claims have the potential to impede your practice, drawing focus and resources away from patient care and crucial healthcare delivery facets. Let us assist you in mitigating and resolving accounts receivable and claim denials, safeguarding your financial stability, reputation, and operational efficiency.
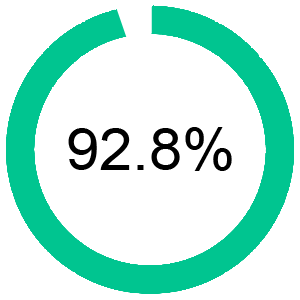
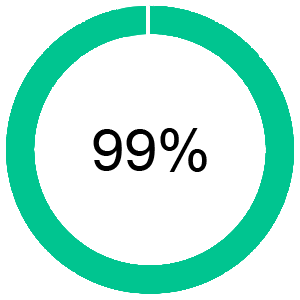
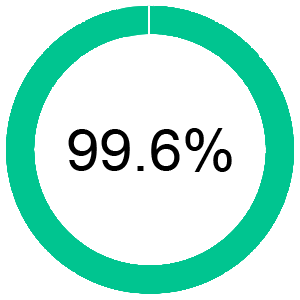
A/R METRICS THAT MATTER
WE MEASURE DOZENS OF METRICS FOR CONTINUOUS IMPROVEMENT
Revenue Realization Date
(Day 30)
Net Collection Rate
(NCR)
Clean Claim Rate
7%
Accounts Receivable
> 90 Days
3.1%
Denial Rate
22 Days
Days Outstanding Revenue (DRO)
THE LANGUAGE OF MEDICAL BILLING
A/R Metrics
Accounts Receivable (A/R) is a key metric to measure the average number of days it takes to receive payment on claims
Clean Claim Rate
Rate of claims accepted by payers without omissions or errors
First Pass Claim Yield
Audits drive the need for precise coding. Even minor deviations trigger legal scrutiny with significant time and energy costs. Many physicians repay funds due to coding errors, emphasizing the importance of accuracy.
Net Collection Rate
Ratio of payments to net charges.
Revenue Realization Rate
Proportion of charges paid within a measurement period of 30, 60, 90 or 180 days.
True Reimbursement Rate
Average payments received against billed charges based on contractual adjustments .
THE LANGUAGE OF
MEDICAL BILLING
A/R Metrics
Accounts Receivable (A/R) is a key metric to measure the average number of days it takes to receive payment on claims
Clean Claim Rate
Rate of claims accepted by payers without omissions or errors
First Pass Claim Yield
Audits drive the need for precise coding. Even minor deviations trigger legal scrutiny with significant time and energy costs. Many physicians repay funds due to coding errors, emphasizing the importance of accuracy.
Net Collection Rate
Ratio of payments to net charges.
Revenue Realization Rate
Proportion of charges paid within a measurement period of 30, 60, 90 or 180 days.
True Reimbursement Rate
Average payments received against billed charges based on contractual adjustments .
STREAMLINED MEDICAL CLAIMS PROCESS FOR FASTER REIMBURSEMENTS
The Claimocity end-to-end revenue solution utilize a blend of AI-enhanced smart technology led by an expert RCM billing team with decades of experience to achieve higher and faster reimbursements while maximizing your revenue cycle operations.
Our software and services reduce administrative burdens and help automate and streamline claims management, payment processing, coding, contracting, credentialing, and compliance to ensure that the clinicians, front office, practice manager, and billing team are always on the same page.
STREAMLINED MEDICAL CLAIMS PROCESS FOR FASTER REIMBURSEMENTS
The Claimocity end-to-end revenue solution utilize a blend of AI-enhanced smart technology led by an expert RCM billing team with decades of experience to achieve higher and faster reimbursements while maximizing your revenue cycle operations.
Our software and services reduce administrative burdens and help automate and streamline claims management, payment processing, coding, contracting, credentialing, and compliance to ensure that the clinicians, front office, practice manager, and billing team are always on the same page.
WE BELIEVE IN REVOLUTIONARY TRANSPARENCY
Your A/R and collections should be fully transparent and readily available.
We provide a full continuum of integrated revenue cycle services and products that supports various sized practices and a wide range of specialties.
The Claimocity medical billing and coding team typically sees a 9-26% increase in collections.
WE BELIEVE IN REVOLUTIONARY TRANSPARENCY
Your A/R and collections should be fully transparent and readily available.
We provide a full continuum of integrated revenue cycle services and products that supports various sized practices and a wide range of specialties.
The Claimocity medical billing and coding team typically sees a 9-26% increase in collections.
Physiatrist and Hospitalist Billing Services for Hospital/Facility Physician Practices
We don’t just offer general RCM services for hospitalists, physiatrists, and physicians on the move, we designed everything we do for doctors on the go from specialized software to exclusive billing with a team that specialized in hospitalist revenue cycles.
Physiatrist and Hospitalist Billing Services for Hospital & Facility Physician Practices
We don’t just offer general RCM services for hospitalists, physiatrists, and physicians on the move, we designed everything we do for doctors on the go from specialized software to exclusive billing with a team that specialized in hospitalist revenue cycles.