Claimocity Claims
Charge Capture and the Revenue Cycle:
A Complete Guide for Healthcare Providers

Here’s a startling fact: Healthcare providers can lose up to 5% of their revenue due to missed charges alone. That’s more than most providers would spend on a charge capture solution. If you’re a healthcare provider looking to understand how charge capture affects your bottom line, you’re in the right place. Let’s break down this crucial step of the healthcare revenue cycle in simple terms.
What is Charge Capture?
At its most basic, charge capture is how healthcare providers record the services they provide and submit them for payment. It is like creating a detailed receipt–every procedure, supply, and service must be documented to be billed correctly. It’s a critical step in getting paid for your work.
Where Charge Capture Fits in Your Revenue Cycle
Charge capture is just the first part of the revenue cycle. Once services are captured and translated into standardized medical codes, they form the basis of insurance claims. When services are properly documented and coded from the start, each subsequent step runs more smoothly. An optimized charge capture process will capture more billable charges, speed up payment, reduce denials, and increase your bottom line.
Your revenue cycle includes:
- Charge Capture
- Claim Submission
- Payment Posting
- AR Management
- Denials Management
- Patient Billing & Collections
- In-App Billing Support
Why Traditional Charge Capture Methods Fall Short
Healthcare providers face many hurdles when it comes to capturing charges accurately and efficiently. Even though Electronic Health Record (EHR) systems have made many parts of healthcare more efficient, charge capture is still a complex task with plenty of room for mistakes. These errors can be costly, and it is essential to identify where improvements can be made to streamline the process and reduce revenue loss.
- Communication Breakdowns: Misalignment between clinical staff and billing teams and inconsistent workflows across different care settings can allow important billing information to fall through the cracks. When departments don’t communicate effectively, charges can be missed or coded incorrectly.
- Coding Complexity: With thousands of CPT and HCPCS codes to choose from, selecting the right codes requires extensive knowledge and attention to detail.
- Human Error: Even with the most diligent staff, manual data entry, and transcription mistakes are inevitable. Something as simple as a mistyped code can lead to claim denials or delayed payments.
- Complex Payer Requirements: Insurance payers frequently update their rules, documentation requirements, and reimbursement policies. Keeping your systems current is an ongoing challenge that requires constant attention and updates.
These challenges aren’t just administrative headaches—they directly affect the financial health of your organization.
It’s Time to Optimize
Stop leaving money on the table. The right charge capture process can transform your entire practice. By implementing these strategies, you’ll streamline workflows, strengthen your revenue cycle, and maximize financial performance:
Start Strategic Auditing
Regular audits aren’t just about finding problems–they’re about preventing revenue loss before it happens. By conducting systematic reviews of your charge capture process, you’ll identify missed charges, avoid under and over billing, and spot opportunities for improvement. Strategic audits will ensure compliance and help maximize your revenue potential.
Leverage Modern Technology
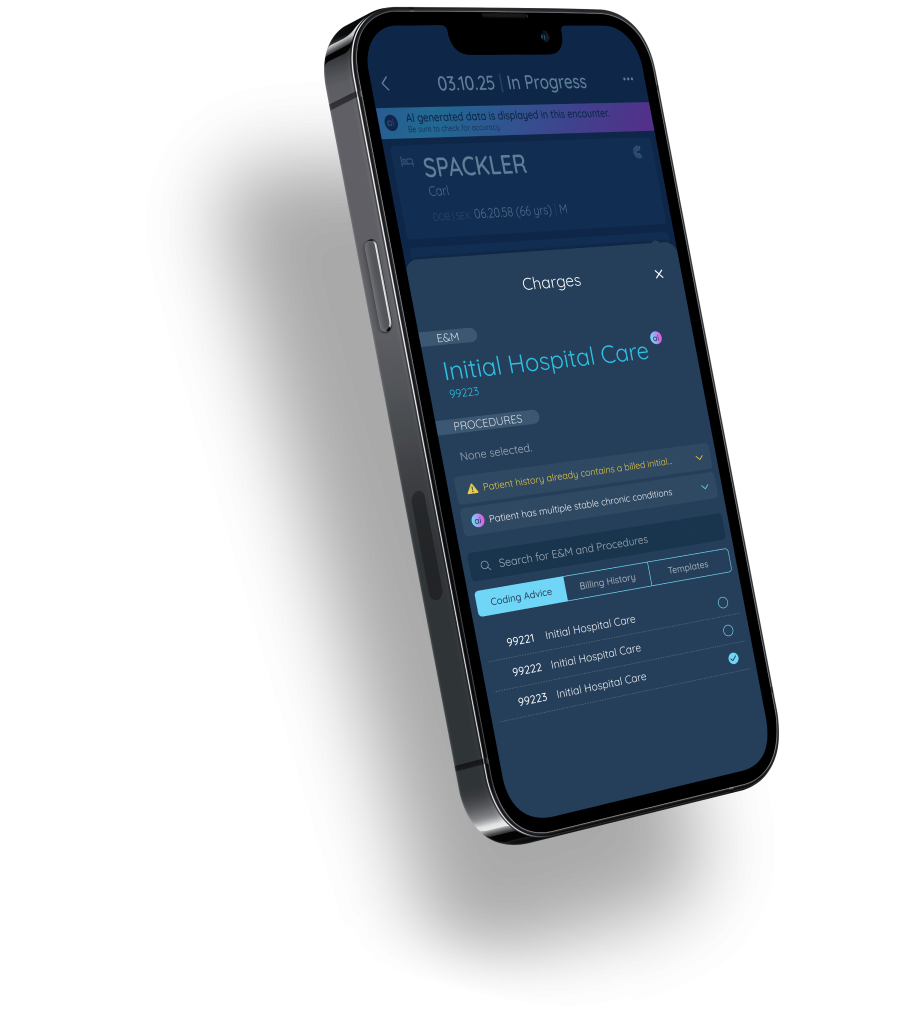
Today’s charge capture technology eliminates the guesswork and manual processes that lead to lost revenue. AI-powered solutions automatically review clinical documentation and suggest appropriate codes, catching potential missed charges before they impact your bottom line. Mobile applications like Claimocity that integrate with your EHR allow providers to document and code services on the spot. No more end-of-day documentation or searching through complex code libraries.
Set Up Your Team for Success
We know your team works hard to keep your organization running smoothly, but great teams need great processes. Make their jobs easier with streamlined workflows that optimize the charge capture process. Clear protocols eliminate confusion, standardized documentation prevents lost charges, and regular training keeps everyone up to date. Efficient processes will boost your bottom line and create confident, engaged teams that consistently deliver better financial outcomes.
Ready to Capture Every Dollar?
Don’t let an inefficient charge capture processes drain your revenue potential. With the right strategies and technology you can capture every billable encounter, make your job easier, and turn potential into profit.
Transform Your Practice Today
At Claimocity, we know healthcare is complex but your charge capture process doesn’t have to be. Our AI powered charge capture will document every encounter and accelerate cash flow. Schedule a demo today to learn how Claimocity charge capture can optimize your process so you can save time and earn more money.
Frequently Asked Questions
What is an example of charge capture?
An example of charge capture is when a doctor provides patient care, like stitching up a wound, and documents the service provided and any supplies used. This information is then converted into a medical code and sent to billing so the doctor can get paid.
What is included in the revenue cycle?
The healthcare revenue cycle covers everything from initial patient registration and treatment, through charge capture and coding, to claim submission and payment processing, and finally collecting any remaining patient balances or handling denials.
What is revenue cycle management?
Revenue Cycle Management (RCM) is the process healthcare providers use to track and manage patient care services from initial appointment to final payment. RCM covers everything from registration and insurance verification to coding, billing, and collecting payments. Effective RCM ensures timely reimbursement, minimizes denials, and optimizes financial performance.
Why is charge capture important?
Charge capture directly impacts a healthcare provider’s financial health–when services aren’t properly captured and coded, providers don’t get paid for their work, which leads to lost revenue.
How can charge capture technology improve the process?
Charge capture technology like AI streamlines the billing process by automating documentation, suggesting accurate billing codes, catching errors before they happen, and helping providers capture every billable service.
How does charge capture fit into the medical billing cycle?
Charge capture is one of the first steps in the medical billing cycle. It occurs after patient care but before claim submission. During this phase, providers document all services performed and translate them into billable codes. It is the foundation for accurate claim submission and proper reimbursement.


