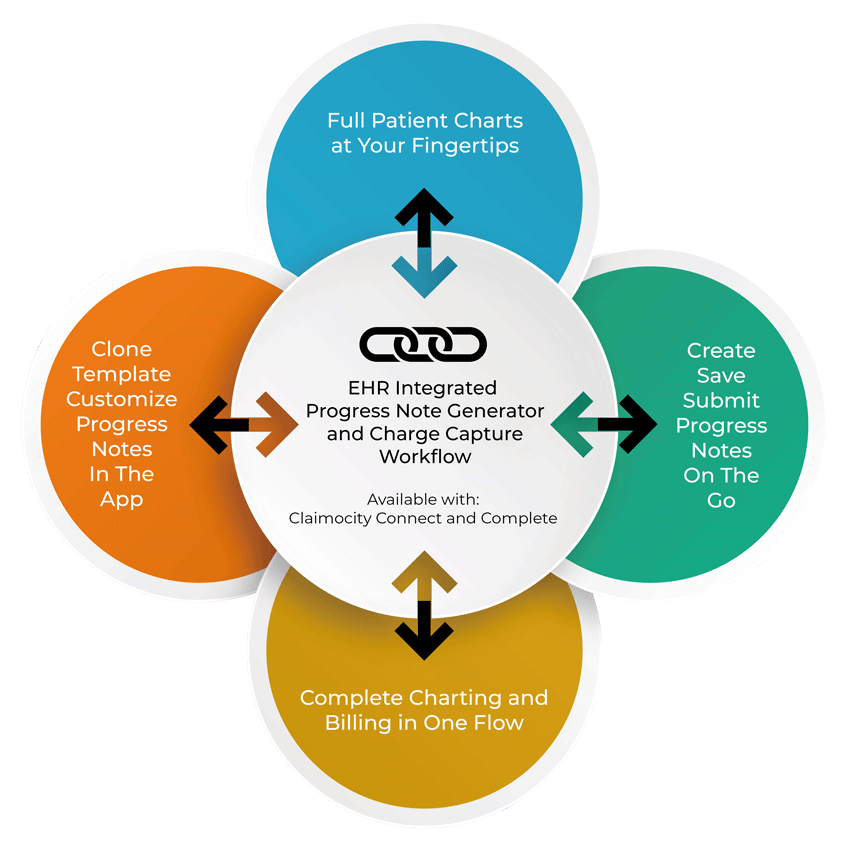
Integrated Clinical Note
Create & Save Post-Acute Notes Within the App

Benefits
- Simplify Billing and Charting in One Fluid Workflow
- Accelerate Progress Note Generation by 68%
- Practice and Provider Level Customizations
- Harness the Power of Smart Cloning and Templating
- Integrate with PointClickCare & MatrixCare
- Design Specifically for Post-Acute SOAP Notes
Designed Exclusively for Rounding
Doctors in Post-Acute Facilities
Effortlessly Connect and Collaborate Across Post-Acute Settings
A Transformative Solution
Experience swift clinical documentation and fulfill billing requirements with our innovative platform. The Claimocity app enables physicians to create, sign, and submit notes directly to Facility EHRs, bypassing integration hurdles.
Eliminate practice-side EHR complexities for hospitalist encounter documentation. Integrate with leading EHR platforms like PointClickCare, Epic, Cerner, and more, ensuring HIPAA compliance and efficient information sharing.
Claimocity's Progress Note Generator Saves 68-73% Admin and Billing Time per Patient
Mobilizing Smart Solutions
- Access the EHR on your mobile device for charting from anywhere
- Combined charting and billing to eliminate redundant data entry
- Quickly submit follow-up notes with charge capture in 30-60 seconds
- Complete initial visit notes and billing in just 3 minutes
- Utilize speech-to-text for hands-free note creation and submission
- Smart syncs retrieve pertinent data from the EHR or census into new notes
- Adapt and clone notes from covering providers to improve care coordination
- Customize templates to meet diverse requirements and contextual needs
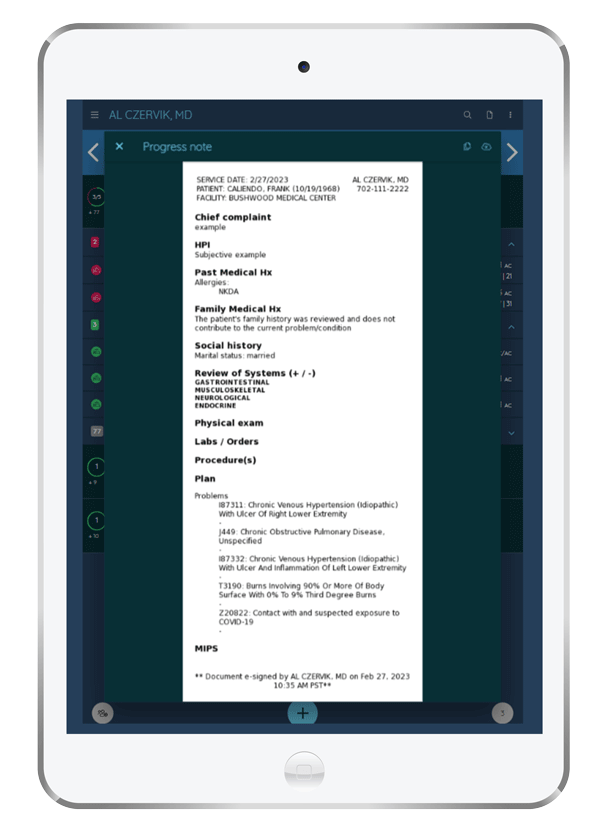
The Smart Physician's Toolbox
Duplicate previous notes within Claimocity, combining and simplifying two daily encounter documentation and billing processes for efficiency. Our note-capture section automatically populates vitals and imports chart elements, supporting various templates. Easily transfer data groups from third-party sources, customize formatting, and establish conditional sections using an AI-driven rules engine. Facilitate note transmission to the progress or miscellaneous section, aligning with existing EHR workflows.
The flexible setup allows comprehensive integration of information before submission. Upon submission, the electronic note is signed, dated, converted into a PDF, and appended to the patient file or electronically faxed as per facility protocols.