Claimocity Claims
HCPCS vs CPT Codes:
A Guide for Inpatient Providers
Navigating the maze of medical billing can feel overwhelming, especially when working across multiple facilities with different systems and requirements. For inpatient providers, efficient billing begins with understanding the two essential coding systems: HCPCS (Healthcare Common Procedure Coding System) and CPT (Current Procedural Terminology). Together, these systems create the standardized language that ensures procedures, services, and supplies are properly documented so you can get paid for your work.
Errors in coding are costly. In fact, American doctors lose around $125 billion each year due to billing mistakes. To avoid becoming part of that statistic, let’s explore the differences between these two systems—and how mastering them can improve your practice’s bottom line.
At a Glance: HCPCS vs CPT
Here’s a quick breakdown of the main differences:
CPT
Purpose: Focuses on medical procedures and services.
Structure: Five-digit numeric codes, split into three categories:
- Category I: Standard medical procedures
- Category II: Performance tracking
- Category III: Emerging technologies
Who uses it: All insurance companies and healthcare providers.
Primary Applications: Medical procedures, services, and diagnostics.
HCPCS
Purpose: Expands beyond CPT codes to include medical supplies, equipment, and non-physician services.
Structure:
- Level I: Mirrors CPT codes.
- Level II: One letter followed by four numbers.
Who uses it: Required for Medicare, Medicaid, and adopted by other insurers.
Primary Applications: Medical supplies and equipment, prescription drugs, and ambulance services.
Key difference: Think of CPT as covering what you do, while HCPCS Level II covers what you use to do it.

What Are CPT Codes?
Current Procedural Terminology (CPT) codes are the industry standard for describing medical procedures and services. Created and maintained by the American Medical Association, these five-digit codes are like a universal language for medical billing. They ensure consistency across providers, payers, and facilities.
CPT Code Structure
CPT codes consist of five numeric digits and are divided into three categories:
Category I: the most common CPT code–Common procedures and services like surgeries or office visits.
Category II: Supplemental codes for tracking and performance metrics.
Category III: Temporary codes for emerging technologies and services.
Examples
- An office visit for an established patient is typically coded as 99213.
- Initial hospital care for a new inpatient is coded as 99221.
- Critical care services provided to a patient in a life-threatening condition are coded as 99291 for the first 30-74 minutes.
Think of CPT codes as telling the story of your patient’s hospital journey—from admission through discharge. Each code represents a specific event in that story, detailing the level of care provided at each step. These codes ensure that every medical procedure and service is described in detail, making it easier for billing teams to submit accurate claims.
What Are HCPCS Codes?
Healthcare Common Procedure Coding System (HCPCS) codes take things a step further. These codes were developed by the Centers for Medicare and Medicaid Services to complement CPT codes and cover the items that CPT codes don’t include, like the tools and resources you need to provide care, such as medical supplies, equipment, and some medications.
HCPCS Code Structure
HCPS codes are divided into two levels.
Level I: Often referred to as CPT-4, these codes align with CPT codes to describe standardized medical procedures and services.
Level II: These alphanumeric codes cover essential items like wheelchairs, bandages, and medications. The letter prefixes help categorize the type of product or service, making identification and billing more straightforward
*There was a level III, but this was discontinued in 2003.
Examples
A-C Codes: Used for transportation services (like ambulances), medical supplies, and some administrative services.
- Example: Surgical dressings needed after an inpatient procedure might be billed as A6203
E Codes: Assigned to durable medical equipment, such as wheelchairs or hospital beds.
- Example: A patient requiring a wheelchair would be billed under the HCPCS Level II code E1234.
J Codes: Drugs administered via injection.
- Example: Insulin injection might be coded as J1815.
HCPCS complement CPT codes. While CPT codes describe what you do, HCPCS codes cover what you use to do it—the medications, equipment, and supplies that support patient care.
Why It Matters For Your Practice
Revenue: Using the wrong code type can lead to claim denials and delayed payments. When you understand which code set to use, you’re more likely to get paid correctly the first time.
Compliance: Medicare and Medicaid often require specific HCPCS codes for certain services and items. Using the correct codes helps you stay compliant with payer requirements.
Efficiency: Knowing when to use each code type speeds up your billing process and reduces the time spent correcting coding errors.
Communication: Standardized codes simplify collaboration between providers, payers, and billing teams and ensure everyone is on the same page.
Coding Simplified
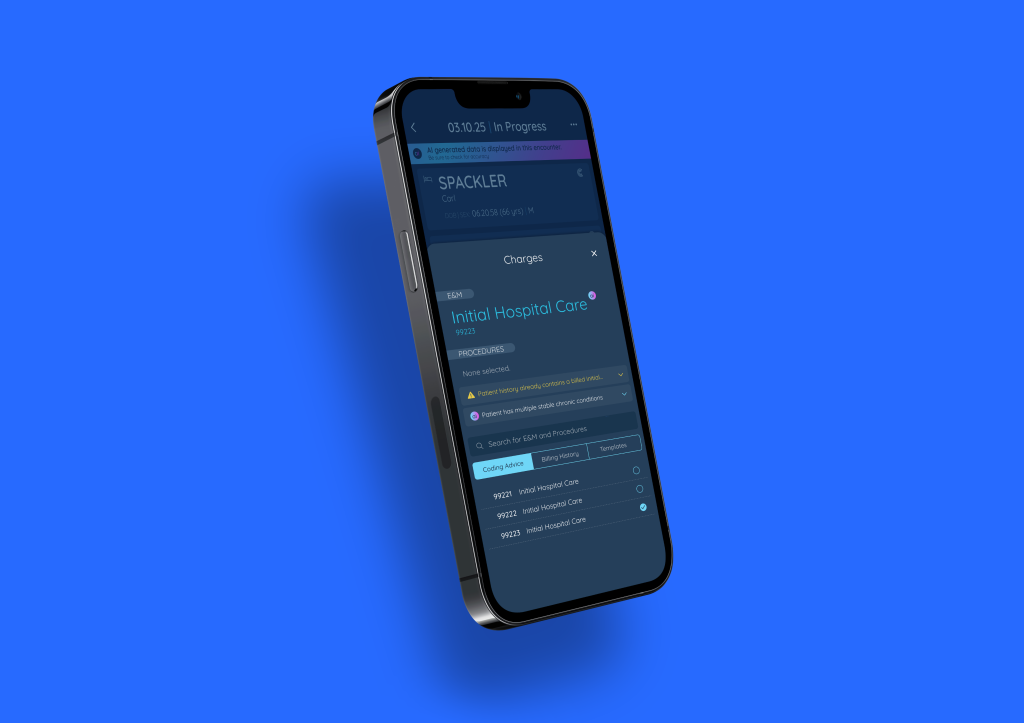
Here’s the thing—you didn’t go through years of medical training to spend hours puzzling over billing codes. That’s where we come in. Our AI Charge Capture solution automatically suggests appropriate codes based on your clinical notes, whether they’re CPT or HCPCS, helping you reclaim your time while maintaining billing accuracy. Our system integrates seamlessly with your EHR, reducing manual entry errors and ensuring that no billable event is missed.
Work Smarter With Claimocity
Understanding HCPCS and CPT codes is just one part of the equation. Claimocity’s all-in-one platform takes the complexity out of billing for inpatient providers. Whether it’s automating your charge capture, reducing administrative tasks, or ensuring compliance, our solutions are designed to help you reclaim your time and maximize your revenue.
Ready to stop leaving money on the table and automate your coding workflow? Let’s talk about how Claimocity can transform your practice.
Frequently Asked Questions
What is the difference between CPT and HCPCS codes?
CPT codes are used by doctors to document medical procedures and services for billing, while HCPCS codes cover additional items such as medical supplies, equipment, and non-physician services. Think of CPT as covering what you do, and HCPCS codes cover what you use to do it. For example, if you’re an infectious disease specialist treating a patient with antibiotics, you’d likely use a CPT code for your consultation (99253) and a HCPCS code for the antibiotic administered (J0696).
What is an example of a CPT code?
CPT codes are used to describe medical procedures and services. For example 01402 represents anesthesia for a knee surgery.
What is an example of an HCPCS code?
HCPCS codes are often used for medications and equipment. For example, A4649 is used for miscellaneous surgical supplies.
Can I use CPT codes for all my billing needs?
No. While CPT codes cover most medical procedures and services, you’ll need HCPCS Level II codes for many supplies, medications, and equipment used in inpatient care. Using both systems ensures you capture all billable items and services.
How do I know which code level to use?
The level of service depends on several factors, including time spent, complexity of decision-making, and extent of examination. Documentation is key—your clinical notes should support the level of service coded.


