Claimocity Claims
Charge Capture Audits:
What You Need to Know

How Audits Can Save Time and Money
If you’re running a medical practice, you might be leaving significant money on the table without even realizing it. We know healthcare providers are already juggling countless responsibilities, and conducting an audit doesn’t seem like the most important thing. Yet studies show the average medical practice loses approximately $125,000 each year due to poor charge capture accuracy. That’s revenue you’ve earned but never collected.
The solution? A strategic charge capture audit. When done right, these audits do more than identify missing revenue—they spotlight workflow inefficiencies, ensure compliance, and create opportunities for improvement in your charge capture process.
Let’s explore how to conduct an effective charge capture audit and discover how AI-powered solutions can prevent revenue leaks before they happen.
What Exactly is a Charge Capture Audit?
Think of a charge capture audit as a health check-up for your medical billing process. It examines how effectively you’re documenting and billing for all the services you provide to patients. This includes everything from initial patient registration to final reimbursement. With so many steps and handoffs between different departments and systems, there are countless opportunities for charges to slip through the cracks.
Where Does Charge Capture Fit in Your Revenue Cycle?
Effective charge capture is the backbone of your practice’s financial health. It’s a crucial part of your healthcare revenue cycle, transforming your clinical experience and patient care into revenue. However, the challenge is that the traditional medical billing process is full of chances for critical information to be overlooked, leading to missed revenue.
Think about your daily workflow. You provide excellent patient care. Your services need to be documented, coded, and billed correctly. With manual processes, charges can be missed, coded incorrectly, or lost between systems. Even the most diligent practices can lose revenue this way.
Why Charge Capture Processes Fail (And Why It Matters)
Most practices lose substantial revenue due to inefficient revenue cycle management. Understanding where these breakdowns occur is the first step to optimizing billing workflow.
People-Related Issues:
Your clinical team is focused on delivering exceptional patient care, but traditional charge capture creates unnecessary administrative burdens:
- Healthcare providers are experts in patient care, not billing. After long shifts focused on delivering quality care, billing accuracy often suffers. This leads to missing charges and incomplete documentation.
- Administrative staff handling charge capture need consistent processes and training to succeed. With high turnover rates and complex requirements, maintaining billing accuracy becomes nearly impossible without the right tools.
Process-Related Issues:
- When responsibilities are spread across multiple departments, accurate charge capture becomes a complex challenge. Without centralized oversight, charges slip through the cracks, and reporting becomes unreliable.
- Many practices operate without standardized charge capture protocols, leaving each department to develop its own methods. This lack of consistency creates confusion and increases the likelihood of billing errors.
- Daily charge reconciliation shouldn’t consume hours of staff time. Yet that’s exactly what happens with manual processes—these essential reviews get postponed or overlooked, leading to lost revenue and delayed reimbursements.
These issues impact more than just your bottom line. They can trigger compliance problems, lead to insurance claim denials, and even affect patient satisfaction when billing errors occur.
But there is good news: these revenue-draining inefficiencies don’t have to be part of your practice. By identifying these common failure points in traditional charge capture, you can take steps toward a more efficient, automated approach that protects your revenue and frees up valuable time.
How to Conduct a Charge Capture Audit
We get it—just hearing the word “audit” can feel overwhelming. But, a charge capture audit is simply a review of your billing process to make sure you’re getting paid for all the care you provide. By breaking it down into strategic steps, you can identify and fix the gaps in your revenue cycle. Here’s how to make it painless and productive:
Start With High-Impact Areas
Focus your initial audit efforts where they’ll make the biggest difference. Complex billing requirements and high-volume departments are the most likely places for revenue leaks:
- Departments with complex services (cardiology, surgery, emergency)
- Areas with frequent documentation delays
- Departments handling expensive procedures or medications
Track Your Progress
Understanding your current workflow is crucial for identifying where charges get lost. Map out your current charge capture workflow from start to finish and look for these common issues:
- Missing or incomplete documentation
- Coding errors and charge entry mistakes
- Insurance information accuracy
- Delays in claims and payments
Audit Early and Often
Don’t wait for problems to compound. The longer you wait to review charges, the harder it becomes to correct issues and capture revenue. The industry’s best practice is to audit charges within 3-5 days of service. This allows you to:
- Catch issues while details are fresh
- Fix problems before claims are submitted
- Prevent denial-related headaches
- Maintain steady cash flow
Get the Right People Involved
Successful audits require perspectives from every part of your revenue cycle. Each team member brings unique insights into how charges flow through your practice. Your audit team should include voices from:
- Financial departments
- IT systems
- Clinical staff
- Billing and coding specialists
What to Expect From Your Audit
With regular, well-executed charge capture audits, you can see exactly where revenue is falling through the cracks in your practice. You’ll get a clear picture of how every process and department impacts your revenue cycle and find practical steps to maximize reimbursements.
Why Wait For an Audit? Stop Revenue Leaks Before They Happen
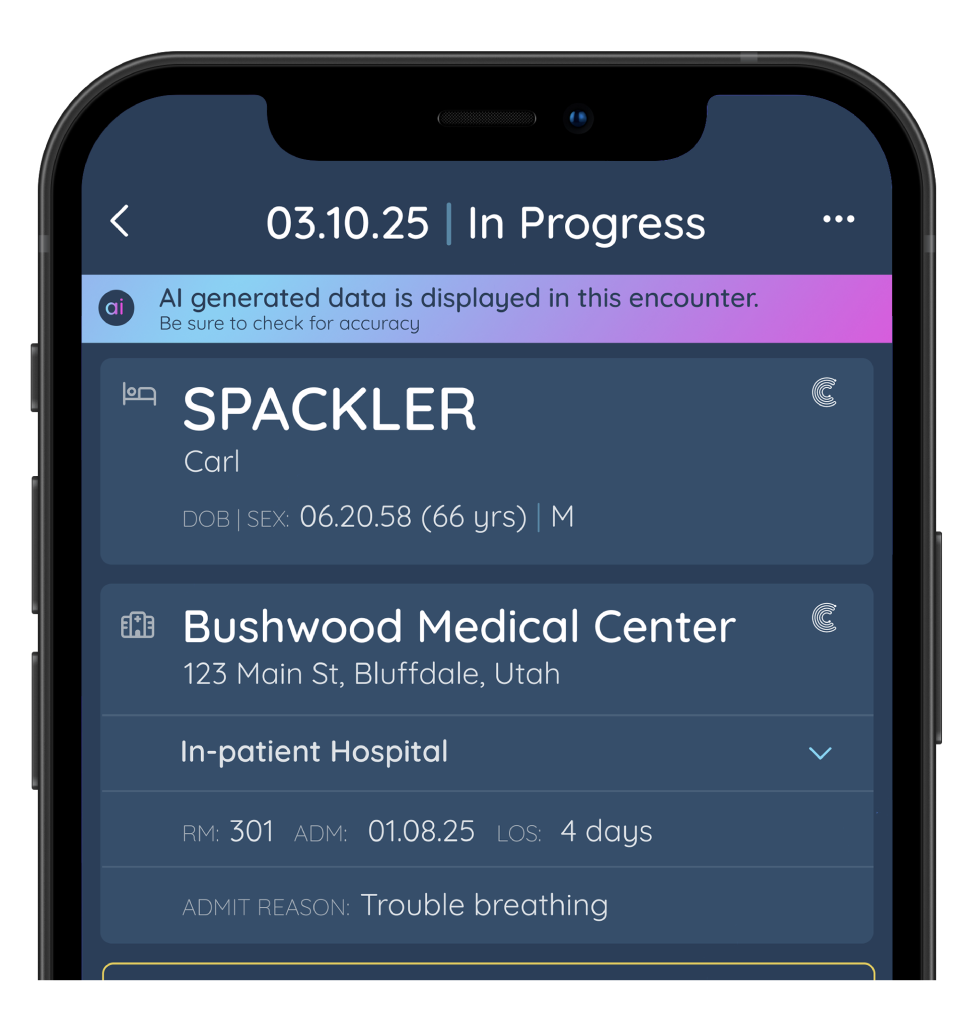
While charge capture audits are valuable and necessary, they are retrospective by design–only finding problems after they’ve occurred. That’s why Claimocity is perfect for healthcare practices that want to get ahead of these issues. Rather than relying on audits to find missed revenue retroactively, Claimocity AI Charge Capture helps prevent revenue leaks from happening in the first place.
Claimocity AI Charge Capture helps achieve the same goals as a traditional audit by working proactively to identify issues by:

- Suggesting appropriate codes based on clinical notes
- Reducing administrative burden and manual entry errors
- Identifying potential missed charges before they occur
- Streamlining the entire billing process
When you integrate Claimocity AI into your daily workflow, you can address many issues that charge capture audits uncover, including missed charges, coding inconsistencies, and documentation errors, before they become problems. This proactive approach ensures you capture all billable events accurately without waiting for an audit to identify and resolve problems.
Are you ready to stop revenue leaks before they happen? Schedule a demo to see how Claimocity’s AI Charge Capture can transform your practice’s revenue cycle management.
Frequently Asked Questions
What is a charge capture audit?
A charge capture audit examines how effectively your practice documents, codes, and bills for patient services. Reviewing each step in your charge capture process will help identify missed charges, coding errors, and process gaps that lead to lost revenue.
What is an example of a charge capture?
An example of charge capture is when a doctor provides patient care, like stitching up a wound, and documents the service provided and any supplies used. This information is then converted into a medical code and sent to billing so the doctor can get paid.


